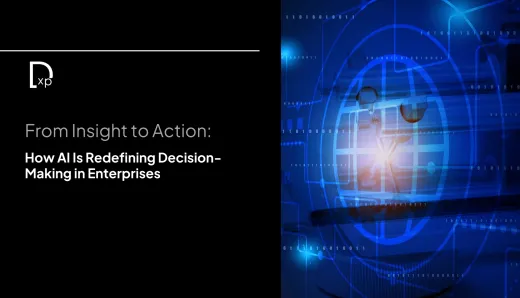
Virtual Reality: A New Comfort in Cancer Treatment
Virtual Reality (VR) technology is making waves in various fields, from gaming to medicine, and its transformative power is now reaching cancer treatment centers. Recently, the University of Pennsylvania’s Penn Medicine Radiation Oncology department collaborated with a virtual reality film class from Penn’s School of Arts & Sciences to create an immersive VR experience for cancer patients about to undergo radiation therapy. This initiative aims to alleviate patient anxieties by allowing them a realistic, behind-the-scenes look into the radiation process, fostering greater understanding and comfort.
For many, cancer radiation treatment is an unknown and often intimidating process. Common questions among patients include the potential discomfort of the radiation, the effect of the radiation itself, and whether the experience of using a face mask for head and neck radiation is tolerable. Through VR, patients can shadow the experience of another patient’s treatment journey, meet key team members involved in their care, and explore the treatment spaces before their first session. This innovative approach seeks to minimize the fear and stress associated with radiation therapy, empowering patients with familiarity and knowledge.
The Power of Virtual Reality
The Penn Medicine Radiation Oncology VR project features two immersive videos, created in collaboration with the undergraduate students of the Virtual Reality Lab course taught by Peter Decherney, a professor of Cinema and Media Studies. These videos were first introduced to lung cancer patients in late 2024 at Penn Medicine’s Perelman Center for Advanced Medicine and are set to expand to other patients in the future.
In the first VR video, viewers enter treatment rooms and meet team members such as medical dosimetrists and radiation therapists, who work directly with patients or manage operations behind the scenes. For example, medical dosimetrist Gabrielle Collinsworth demonstrates how treatment plans are developed, while medical physicist Austin Kassaee ensures the radiation is administered correctly. Radiation therapist Angela Natale explains the rationale behind radiation masks and tattoos, a crucial part of radiation for head and neck cancer patients, easing concerns over the safety and purpose of these elements.
The second video allows patients to follow a former patient, Cindy Olson, on her journey through the Roberts Proton Therapy Center. Viewers gain insights into what to expect at every stage, from the initial consultation to the treatment room. Olson shares her experience with the radiation mask, noting how it gave her a sense of security and comfort, helping her stay calm through the process. Her story also emphasizes the community aspect of cancer care, as she describes the supportive interactions with fellow patients in the waiting room.
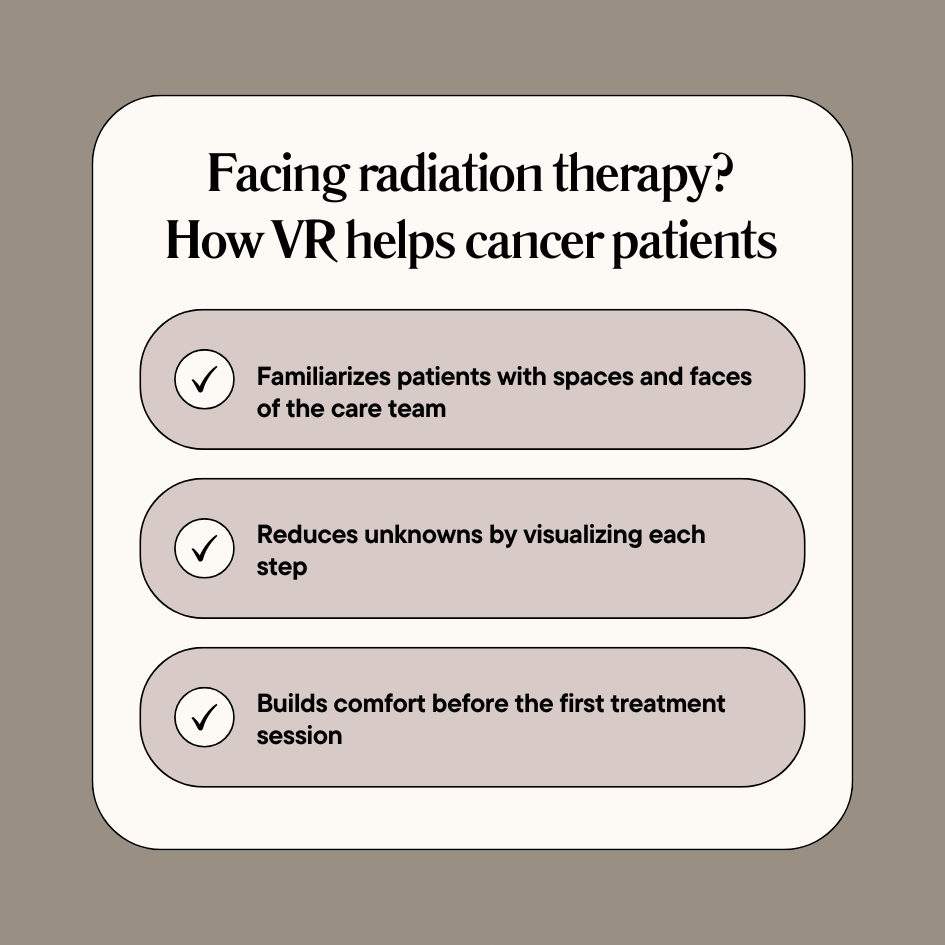
These VR experiences allow patients to see the compassionate care that awaits them and get a feel for the medical spaces they will soon enter. By “shadowing” another patient, individuals can envision themselves in the treatment process, gaining familiarity and easing fears of the unknown.
The Virtual Reality Experience
In this context, Virtual Reality is comprehended as not merely images but stepping into an experience. It offers immersion levels that certainly surpass traditional patient education, making it rightly attractive for preparing the patients for the unknown frightening journey. Peter Decherney, lead instructor of the project, opines that this immersive medium allows them to "actually feel the surroundings", providing that degree of empathy and understanding that neither words nor images can match.
360-degree camera footage used by students in the Virtual Reality Lab class place the viewers right inside the setting; they would be compelled to walk independently and explore the rooms and environments. This extreme level of immersion offers control and insight, bringing deeper experiences and bridging a gap between the patients and the intimidating process of radiation.
From a patient-care perspective, the project extends beyond its primary purpose of education; it demonstrates the empathy and dedication of the medical team. As Fern Nibauer-Cohen, Senior Director of Patient Engagement, observes, each team member's passion for their work shines through, conveying not only expertise but a genuine commitment to patient care.
A Collaborative and Educational Endeavor
The creation of these VR videos has not only benefited patients but also provided an invaluable learning experience for Penn students. For many film students, working closely with a medical department and capturing real patient experiences was a unique opportunity. Biophysics major Amalya Knapp, the lead interviewer in Olson’s video, shares how she witnessed the collaborative nature of medical care, describing it as a “team effort.” The students’ interactions with doctors, nurses, and patients added a layer of depth to their academic journey, exposing them to the realities of compassionate healthcare in practice.
This partnership is also an example of interdisciplinary collaboration at Penn. Inspired by a 2023 article about the VR course, Nibauer-Cohen reached out to Decherney, recognizing the untapped potential of joining forces between the School of Arts & Sciences and the medical field. The weekly meetings between students and medical staff allowed a unique exchange of knowledge and perspective. While students brought creativity and technical skills, the medical team provided real-world patient care insights, resulting in a truly collaborative product that impacts both patient lives and student education.
Broadening the Horizons of Virtual Reality in Medicine
Virtual Reality’s applications in healthcare extend beyond radiation preparation. As a transformative tool, VR has been integrated into various medical training, treatment, and patient education scenarios. In Penn Medicine Radiation Oncology alone, VR is used not only to reduce patient anxiety but also in clinical training and medical education. Under the guidance of radiation oncologist Dr. William Levin, VR is incorporated into anatomy courses, enabling medical students to “enter” organs for a more detailed understanding of anatomy.
Beyond anatomy lessons, Levin is exploring VR’s potential for stress reduction among patients through guided breathing exercises in virtual environments. These exercises offer a moment of calm before radiation treatment, showcasing VR’s versatility as a tool for both psychological support and technical training.
Influence of Virtual Reality on Patient Care
The impact of Virtual Reality on patient care lies in its ability to bridge knowledge gaps and offer comfort in uncertain times. By allowing patients to virtually experience medical procedures, VR reduces the fear of the unknown, making treatments less daunting. Patients can understand the purpose of each step, from the radiation mask to the tattoos marking radiation placement, alleviating some of the anxieties associated with these unknowns. Furthermore, by fostering familiarity with the process, VR gives patients a sense of agency, enabling them to enter treatment with a calmer mindset.
For the medical staff, VR is a means of showing empathy and compassion in a new way. As Nibauer-Cohen highlights, team members were able to express their dedication, letting patients see that they are in good hands. The immersive experience reinforces trust between patients and their care teams, strengthening the patient-caregiver relationship.
The Future Ahead
This initiative by Penn Medicine Radiation Oncology and the Penn Virtual Reality Lab showcases VR’s capability to create meaningful, human-centered experiences that change how patients and providers approach medical treatments. The project also emphasizes the importance of interdisciplinary collaboration in advancing patient care.
Through projects like this, VR has the potential to redefine patient support and education across numerous medical fields. In the future, more hospitals and treatment centers may adopt VR as a standard practice for preparing patients for complex procedures, helping them feel informed, empowered, and less apprehensive about their medical journeys.
For those interested in staying at the forefront of innovation, subscribe to our newsletter. Stay informed on the latest advancements in the digital world and gain insights into the transformative power of technologies.
FAQs
1. What is the purpose of using VR for radiation therapy patients?
VR helps patients understand the radiation process, easing their fears by providing an immersive, behind-the-scenes experience before treatment.
2. How does VR help reduce anxiety for cancer patients?
By letting patients “shadow” a treatment journey, VR allows them to see treatment steps and meet the care team virtually, which reduces uncertainty and fear.
3. Who can benefit from the VR radiation preparation experience?
Any cancer patient undergoing radiation therapy, especially those feeling anxious about the unknowns of treatment, can benefit from VR.
4. What will I see in the VR experience for radiation therapy?
The VR experience includes guided tours of treatment rooms, introductions to team members, and explanations of processes like radiation masks and tattoos.
5. Where is this VR program available for cancer patients?
Currently, Penn Medicine’s Radiation Oncology department offers this VR experience, with plans to expand access across more treatment centers.